Aimee was able to facetime while awake with her siblings. 😍 Otherwise, no new news. The team gave her a saline bolus today to see if it will help with the vomiting issue. I anticipate a quiet day tomorrow too as the weekend is usually pretty slow.
10.30.21 Trach floor 4
Aimee was able to facetime while awake with her siblings. 😍 Otherwise, no new news. The team gave her a saline bolus today to see if it will help with the vomiting issue. I anticipate a quiet day tomorrow too as the weekend is usually pretty slow.
10.29.21 Trach Floor 3
Best, most important part of today, Aimee has been alert! She got up in her wheelchair for the first time for about 10 minutes and she watched a movie for the first time too! She is still struggling with lots of coughing and some vomiting despite having both the gravity drain and suction drain from her stomach, but seeing her alert has been a balm to my heart after this long month.
Okay, she didn’t enjoy the wheelchair and transfer at all, but she did it.
The movie was much more appreciated.
Overall not much else to report today. Working out some details for next week. Monday she has her first trach safe, which is a sedated scope procedure to check on her airway.
I had a visit from one our favorite ICU nurses today. She stopped by to see us and give me a hug. Hugs are a rare and precious gift right now.
10.28.21 Trach floor 2
Nearly forgot to write a quick update today. Aimee is stable and settling into the new unit. This is an area of the hospital we have never stayed in before, but from our understanding, aside from the PICU, this will be where we stay from this point forward. New faces to meet and new rapport to build. We do recognize a few, some of the RTs from previous stays and our MCC team will some of them be familiar. It takes a couple weeks to really build trust with the new unit though, so it will be a bit of finagling til then. 
The new attending gave me a very pessimistic expectation of how long our stay would be. He said that it would take us several months to get back home. We are hoping that is not true, but do know it will be more than one month more for sure. The gut issue is our real unknown wildcard.
GI did stop by today and they still have not been able to communicate together with general surgery and our primary GI doctor. Essentially they told us to hold tight until Monday and make no changes. We are building some serious patience muscles.
10.27.21 MCC Trach Vent Floor!
I came back down this afternoon and had a peaceful afternoon transitioning care, discussing this week with Ed. Then this evening, the ICU team released Aimee to the Medically Complex Care team on the Trach Vent Floor! She just got settled in her new room (forest 3.307). This is a huge step forward after nearly 4 weeks in the ICU. 









While we are so thrilled with this step forward where we get to be participants in her care again, we are concerned about her gut function. The respiratory situation is a matter of time and training, so that will proceed over the next few weeks. The gut… we still have hope that she will return to her ability to be fed via j-tube, but are concerned about the difficulty that she has been having without NG suctioning and the partial obstruction. If she can return to her previous function, will she be frequently dealing with blockages? Will she be able to get back to comfortable digestion without distention and vomiting? If she doesn’t return to function, she will have to go home on TPN. We are not yet in the place where we have to consider these options, but has started to come up in discussion with different team members. We are still waiting to hear back from the general surgery/GI discussions on what steps to take next.
In happy news, I enjoyed a few days at home doing “normal” life, school, snuggles, diapers, milking, and laundry. It was good, though so hard to be separate. I never want to leave home and I never want to leave Aimee here. 💔
10.26.21 ICU 35
Guest blogger #3
When we transfer to the Trach/vent floor, we will be under the MCC (Medically Complex Care) team instead of directly under pulmonary, although they will still be consults for Aimee’s care. This move is because of the continued bowel issues, MCC is better suited to handle this in conjunction with the new Trach.
Aimee spiked a fever this afternoon and they took blood cultures to check again for infection. With her central PICC line they are very cautious and quick to want to rule out an infection.
The G.I. consult came by this afternoon. Not our normal doctor and the team that I was excited about getting all of their inputs, but just the on call GI doctor. One of the most frustrating things about being inpatient at the hospital is that you don’t see your normal doctor, you only see who is on call that week. The doctor came in with an answer to a question that we had asked last week, which we already knew the response to and she wasn’t able to really answer anymore additional questions. She is going to go back and talk with her colleague to hopefully gather some more information. Until then we wait ….
The ICU attending that we have for this week has thanked me multiple times for being patient with them as they try to figure out Aimee’s gut. But really I thank them for being willing to be patient with Aimee. Sometimes I think people get impatient with how long it takes for her body to respond, so I appreciate the willingness to give her time to respond and not just give up on her gut function returning.
In good news, I do feel like there has been some increased output and also air in her ostomy.
I did get a moment when Aimee was awake and caught her looking at me. I feel like the moments of Aimee’s bright eyes and glow have been limited in these last couple of months so I cherish these times when I get to see into her eyes and she recognizes me. I pray that through all these tough moments for Aimee that we are able to restore her joy and glow. She has impacted so many along her journey including myself. I don’t even know what our lives would look like without Aimee’s impact, but I’m so thankful that we have been entrusted with her care.
10.25.21 ICU 34
Guest blogger #2
Visiting with Pulmonary this morning, they were happy with how Aimee was responding to her current vent settings. We are working with respiratory therapy to deal with some of the physical setup of the vent to handle the increased secretions without clogging the exhaust portion. The current vent that she is on is so new that they are still working through some of the bugs.
Today I got some hands-on training for doing the trach care that will need to be done daily. This is part of what we will be trained before we are allowed to go home. It feels good to finally be a part of some of Aimee’s care. We are so used to doing all of it when we’re at home, it feels weird not to do it here.
ENT and wound care came by to check on Aimee. They are both happy with how her stoma and Trach site look. General surgery also stopped by to talk about Aimee’s narrowed/partially blocked bowel. It was the original surgeon who removed the bowel obstruction and also had consulted with 2 of Aimee’s primary GI doctors prior to surgery. Her plan is to round back with them again and discuss what the right plan is for Aimee. A couple of options are either a scope of her small intestine with possible biopsy or an MRI to find out more about the narrowed bowel. It makes me feel so happy to know that the doctors who know Aimee the best are going to be putting their heads together to come up with a game plan.
Today has been a fairly quiet day for Aimee. Thankfully no vomiting. That being said her NG tube has been on suction, which I believe is reducing the pressure and discomfort in her stomach. So although no progress has been made, at least she is comfortable.
10.24.21 ICU 33
Mystery guest blogger ;)
Not a great day today. Had some episodes of throwing up this morning. Her belly was pretty distended this morning until her NG tube was moved back to suction. Following the episodes this morning have a few hours of pretty distressed including shaking hands and high heart rate. Needed a few different doses of medication to break the cycle and calm her back down.
The ICU team is in continued talks with the general surgery and G.I. teams. We are waiting to hear back from G.I. after reviewing the CT scan done on Friday night. Biggest question seems to be what is causing the narrowing of the small intestine. ICU team is taking some stool samples to rule out some possibilities while we wait for GI’s response.
Today Rosa went home to be with the other four kids and take care of the home duties. It is always so difficult to leave Aimee here at the hospital especially when things aren’t moving in an upward direction and seeing her in distress. Rosa does such a fantastic job here taking care of Aimee, but she needs rest and recovery time. She has basically been here more than 3 weeks straight with only a brief 12 hour break.
I wanted to thank all of you whether known or unknown for loving on my family during this time. Each one of us has felt the love and compassion that you have for us and for Aimee. It is truly remarkable to see how far reaching the love and care for our family is. We are so appreciative of our village that helps us care for Aimee.
10.23.21 ICU 32
I had a special guest today join me for a rainy afternoon walk. One great benefit of being in the ICU is the nursing coverage. Getting an hour break to go outside for fresh air is possible and encouraged by some of the wonderful nurses. We haven’t taken advantage of it up to this point, but as Aimee becomes more stable, we have felt more comfortable taking this respite. 
Aimee’s CT scan results came in late last night after I posted. She has a sort of partial blockage in her small intestine. Basically an area of her small intestine that is narrowed and inflamed. It is not completely blocked and does not need another surgical intervention right now. We haven’t been able to talk with GI yet, but at this point, per general surgery’s recommendation, we are staying the course of TPN nutrition, as well as, NG rotating back and forth between gravity and suction. Her abdomen is still very distended.
Respiratory wise she is doing well. She is tolerating her new vent settings and treatments are effective for clearing her out.
Tomorrow I get to go home for a couple of days to be with the younger 4 kids. There is no perfect place to be until we are all together again. The best Ed and I can do is switch back and forth. Very thankful for family watching the younger kids each weekend so that we can have a night here together in Aimee’s room.
10.22.21 ICU 31
Aimee just got back from another abdominal CT scan. It has been an all day affair. She only had her central line and no peripheral IV access left. For a CT they need a 20 gauge IV for contrast and Aimee is not an easy access. As her day nurse said, “She has angel hair pasta veins.” After several nurses and many pokes, the IV team with ultrasound was called. Success!
We also had to pump her already swollen belly full of contrast, which was a very uncomfortable process. Once we navigated the hospital for our field trip, Aimee was shaking so badly that we had to bind her up to take the scan. :(
She is now back in her room. She still needs trach care and a new packing in her abdominal wound, but the nurse kindly agreed to give her a break for a couple of hours. She is calmed and falling asleep now.
Her post-surgery illeus in combination with her vent adjustments are the remaining obstacles keeping her in the ICU now. The team expects to have the vent settings all settled by Monday. We will see if we can get the illeus resolved by then so that we can take that big step forward of discharging from the ICU. Tomorrow will be 21 days here.
10.21.21 ICU 30
Not a lot of progress today overall. Aimee is tolerating the new vent, though it looks like the settings will still need a few more days of tweaking to get them figured out. She has some loss of lung capacity from the transition putting her at less pressure than she should be. Different machines have different software and they don’t directly correlate. They plan to spend the next several days make adjustments to her settings here in the ICU. In the mean time she is needing some additional respiratory clearance.

GI wise, she hasn’t been vomiting much, but this afternoon and evening her stomach has started to become distended again. She has remained on NG suction most of the day. No progress there. Her wound continues to be packed twice a day and is making slow healing progress.
Since she can’t use her digestive system currently, all of her meds have had to be given by IV over this past few weeks. One of the difficulties with this is that many of her regular medications do not have an IV form. Neither of her seizure meds do. So they have her on a different medication that is very effective for her type of epilepsy. The downside is that it is difficult to regulate the dose. Despite having been at a good level several days ago, today when they took bloodwork it was nearly undetectable. They had to give her a large loading bolus and then raise her dose by 50% more. This has helped to alleviate some of the neuro symptoms, particularly the full body clonus type movements, we had been seeing over the past two days.
The wonderful news of the day was for me. I was able to go outside for a walk. We had the same day nurse for the last 4 days and her second patient was discharged from ICU today. She stayed directly with Aimee and I walked up the road to the trail. It was such a restorative act to walk through the snowing leaves of autumn.
10.20.21 ICU 29
Good news, last night at evening rounds we were able to convince the team that Aimee desperately needed a break. They turned the NG suction back on and have only turned it off for short periods today. Much less vomiting. They are changing their strategy to focusing on respiratory and waiting on GI function.

In general she has been very agitated and shaky, but that may be due to the fact that she now completely off of pain, sedation, and anxiety drips. :) She also is just so tired from some level of ICU delirium. I am praying that her neurological system will calm so that she can get good restorative rest.
To that end, today Aimee was moved to a new style of ventilator that she could use out of the ICU. They are still optimizing settings, but she did well with the transition so far. It is called the VOCSN. It is a Ventilator, Oxygen condenser, Cough Assist, Suction, and Nebulizer all in one machine! It was just recently designed in our area.
In general she has been very agitated and shaky, but that may be due to the fact that she now completely off of pain, sedation, and anxiety drips. :) She also is just so tired from some level of ICU delirium. I am praying that her neurological system will calm so that she can get good restorative rest.
We got the results of Aimee’s bone scan today. She has another fracture in her right leg, but it was a less severe one that is nearly healed. We are remembering that she was sensitive to her right leg being moved for a couple weeks back in late August. :( ugh. That is 2 fractures within a 2 month time period both in her legs. It doesn’t change what we will do right now, but it does affirm our plans to do bone infusions and to be even more careful about how her extremities are moved.
10.19.21 ICU 28
Tough day today. Aimee has been so nauseous and uncomfortable, vomiting frequently. I’m trying to get the team to turn back on her intermittent NG suction at least for the night. She hasn’t slept in 2 days now and she is worn out by the day today. She had a full body bone scan this afternoon and the attending is convinced that is why she has been sick. Just from the activity. I’m okay pushing her body a bit, but at this point, she needs rest. :( praying that I can convince them to give her a break tonight and try again in the morning.
The General Surgery team is ordering new abdominal x-rays to make sure everything is still okay in there. They are also consulting back with GI to see if there is anything we can do to help her digestive tract to wake up.
10.18.21 ICU 27
You did not come here to read my expressions of thankfulness I’m sure. I have already expressed this sentiment. Yet, there are feelings of kinship we have with each person who has been supporting us. At risk of sounding melodramatic, I want to try to explain again.
Through the years we have lost friends. We have missed countless gatherings. We have lost dreams. We have rebuilt an idea of what our life would look like. It has for the most part been isolating. We have chosen to link arms with each other and to grow together where we are. It has been worthwhile to care for Aimee and our family.
While we have been dragging ourselves through this past few weeks, so many people in great love and kindness have come around us. Long ago friends, family members, even some distant acquaintances, have each just picked up a corner of our load and walked with us. I’m not sure I can paint a picture for you of how this feels in our hearts. It makes me weep. Ed and I have been teammates with encouragement from others for over 12 years. Yet right now and through this dark couple of weeks, we have heard many cheerleaders who have identified themselves in word and in action as part of Aimee’s team. There are no words to express this team growth, except to say that we are so grateful. And you have made our days lighter just by your recognition of the importance of treasuring, of fighting for Aimee.
Speaking of Aimee, she has really stabilized over this past couple of days. Her room is full of peace. Her symptoms of sepsis are receding. Her quick pneumonia treatment has been effective. She is still sounding coarse and diminished, but her lungs are staying strong with lots of respiratory therapy. She is nearly off of anxiety and sedation meds. She had one more pain med taken off today. They also turned off the suction from her stomach. I will say that she is not comfortable at this point. Her belly is becoming more bloated with fluid, but so far no vomiting. If her stomach and small intestine would just wake up enough to process her own stomach acid, we could move to the next step.
Today we made several plans. I met with a wound care specialist to make a plan for each of the areas of concern. We made a plan with Urology for the future for how to bring in a sterile urine sample from home. We took steps in the plan to have bone density infusion done by getting a dental exam and x-rays. We made a plan to have a body scan done to rule out other fractures. We made a plan with PT to adjust her wheelchair and discussed how to stretch her lower extremities safely to avoid factures.
We also discussed with the medically complex care team the transition process of getting Aimee moved from the ICU. There is a unit that is a step down from here, but higher level than acute care. It is the medically complex trach vent unit. It is set up very similar to ICU, but the specialized nurses cover 3 patients each (ICU it is 1-2 patients, acute care is 4-5). Once in the next unit, we will be able to participate in her care, being trained officially in a classroom and unofficially at bedside. At this point Pulmonary will not sign off on her leaving the ICU, but we feel that we are getting closer. Aimee has been moved from one-on-one nurse care to two patients to one nurse. We are making progress!
10.17.21 ICU 26
Nice quiet Sunday. Aimee made some progress in using less pain medication and getting a better, more comfortable respiratory routine. Her abdominal wound is continuing to be packed twice a day, but is decreasing in size. She had her foley catheter removed. A small amount of ostomy output started, which is very encouraging. Unfortunately, we found multiple skin issues today, blisters under her trach, a pressure sore and some split skin. One of the difficulties of being so restricted and difficult to move lately. Over the next couple of days they will slowly start weaning her off of sedation and anxiety drips. 
Ed went home to be with the younger 4 kids today. Both ends of this are so much easier to do together as a team. 💔
10.16.21 ICU 25
I got to spend last night and this morning at home with the younger 4 kids. It felt good to be home. Came home to a surprise package from a friend from afar with books and tea and activities. It was just so sweet for the kids to feel special and loved. Being home in a little bit of normal routine is such a blessing. 



Today the team turned off Aimee’s pain drip. They are leaving the anxiety/sedation at about half for now. We wanted to focus on cutting back on the medications that interfere with GI function. At this point, the ng is still to suction and it is pulling ALOT of fluid from her stomach, which means her small intestine still isn’t moving. Her ostomy has next to no output and she is still on TPN with IV meds. The first goal will be to have more ostomy output so that we can turn off the suction.
Ed met with Pulmonary a couple of times, PT, General Surgery a couple of times, and Urology while I was gone. Long and short of it, we will be in the ICU for awhile still before we can move to the trach vent floor. She needs to be more stable before she can be released from the ICU. They will not be comfortable with us moving until she is successfully proven on a portable ventilator and until she has made significant progress towards enteral nutrition. She won’t be put on a portable ventilator until she is weaned off of sedation meds and makes progress with her gut. She can’t make progress with her gut until we get her off of the big pain meds. Phew.
Overall Aimee is much more comfortable with the new trach size. She is still having some panicked events, still having neurological symptoms of distress, but they are decreasing. She is fighting a lot of secretions and oxygen saturation issues as she adjusts to less pain meds. It is a tricky transition.
Now that the kids will be back home, Ed and I will be rotating schedules between home and hospital. Thank you to each person for your support through this past 2 weeks. Thank you to each friend who has sent us room service gift cards. Thank you for each message and email and comment. Thank you so much to our many different family members who have helped or plan to help with the younger 4 kids. That is the biggest deal to have them feel safe and loved through all of this. Thank you to each of you for loving on us in your different ways. You have helped us to carry forward and to focus on advocating for Aimee. Thank you for being on Aimee’s team. Please continue to pray that she would stabilize and make significant progress towards healing.
10.15.21 ICU 24
Aimee made it to her first trach change! This is wonderful because she no longer needs to be on fresh trach protocols and this new trach is a longer more comfortable fit for her. 
Child life brought in a stuffed animal with a trach and some coloring pages of animals with trachs for me to bring home to the other kids.
Now that she is off of fresh trach protocol, the team will start weaning her off of her pain med drips and her sedation drips today.


Child life brought in a stuffed animal with a trach and some coloring pages of animals with trachs for me to bring home to the other kids.
Now that she is off of fresh trach protocol, the team will start weaning her off of her pain med drips and her sedation drips today.
Here are her leg x-rays from a few days ago that show her broken bone. 😩 I have been talking with Palliative care and MCC about this and they have both really encouraged me that this sadly very common in complex kids. More often than not there is no known event that caused the fracture, but it is most commonly in the long bones of the body.
10.14.21 ICU 23
Good news, the severe nystagmus and clonic jerks Aimee is having are not seizures. I haven’t talked to Neurology yet, but at least we won’t have to increase seizure meds.
We met an endocrine doctor this afternoon. She ordered a bunch of blood draws to check hormone levels and nutrition levels. We will meet with the skeletal health clinic once Aimee is stable to talk about bone infusion therapies, but for now there may be some hormone support or supplement support that we can give to help her heal the current fracture. Along with that we will have to be very careful from now on when we do her care to not put stress on her bones particularly during transfers, positioning, stretching, and blood draws/IV attempts. I still can’t believe that her femur is fractured.
Tonight the nurse did a new CBC and Aimee’s hematocrit and hemoglobin are both decreasing again after a few days with slightly improving levels. She has been very anemic the whole time we’ve been here, but it is disappointing to be going backwards in her different blood test results today. They are preparing to give her a unit of blood right now.
Overall Aimee is having a calm evening with no increase in respiratory support needed. She has had a couple of mucous plugs today, but once those were cleared she has been doing well respiratory wise.
Tomorrow I get to see the younger 4 kids for the first time in 2 weeks. 💛 Looking forward to leaving the hospital for a night and snuggling them all, but also heartbroken to leave Aimee and Ed here. This is going to be a long, tough road.
Speaking of which, a few people have asked how they can help us. It is hard to think on the spot, so I haven’t answered well. Ed and I sat down tonight and thought about what would help. Thank you to each of you who have already blessed us in different ways. Here are some ideas that would be so appreciated:
-Costco gift cards for gas and for prepared meals
-Hospital room service gift cards
-Starbucks gift cards
-Activities or cards in the mail for the younger kids
-Messages to me or phone calls to Ed to let us know you remember us
-Audio messages to Aimee that we can play for her to hear
-Prayer for each member of our family. This has been a hard 5 months and there is much more to come. It is very difficult on each of us in different ways.
10.14.21 ICU 22
After a fairly quiet day yesterday, today came in more dramatically. The team had an x-ray done in the wee hours of the morning (about 3:45) and noted that there increasing indication of pneumonia in her left lung compared to yesterday. They had been noting all day yesterday how diminished her lower left lung sounded. Her sepsis markers in her blood have increased again significantly. Her fevers have continued. They are starting her on a broad antibiotic that would cover that and the growth from her abdominal incision infection while they wait for the tracheal secretion labs to come back. Today her secretions have increased and appear yellow. So far she is stable as far as respiratory support is concerned.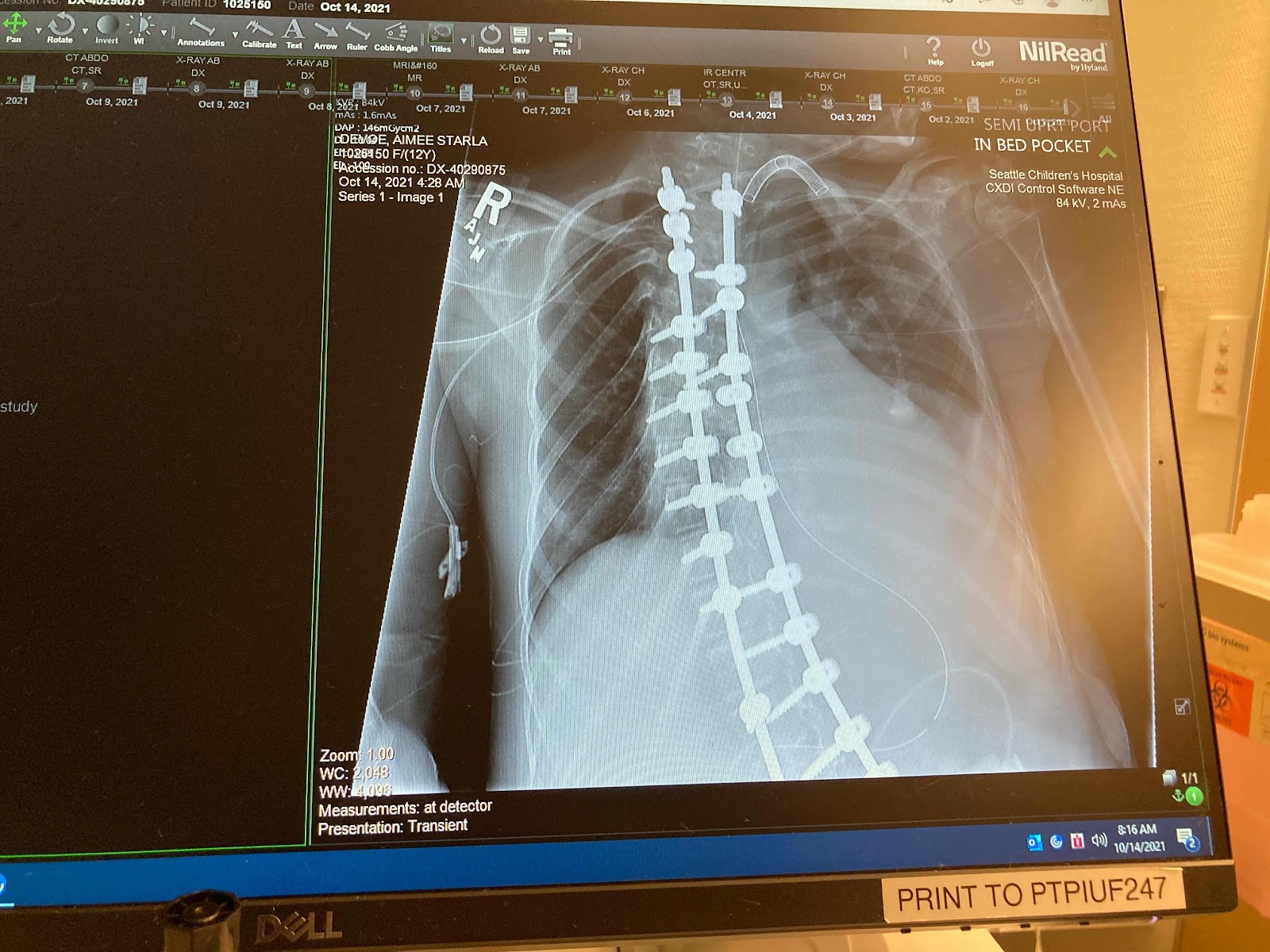


She is currently having an EEG done as the episodes that she was having two days ago have started back up again. Currently they are only happening when we reposition her thankfully, but the neuro team would like to see if they are seizures.
10.13.21 ICU 21
After this morning’s scope they determined that a different type of trach is needed. This one is slipping up and forward easily which is pressing against the trachea and triggering increased neuro symptoms. The hope is to keep her sedated enough to make it to Friday and change it out. If she can’t make it, they would have to change it early causing trauma to the area. So far the change in meds has kept her much more sedated and we have only seen whispers this afternoon of distress.
We did speak with Neurology and if we see the same activity continuing again they will bring in electrodes and hook her up quickly to EEG to decide if it is seizures.
Today we also met with Ortho to get a better fitting leg brace. They discussed her osteopenia condition and the possibility that her GI issues this year may have caused her to absorb less nutrition. When we met with GI, they recommended connecting with Endocrine about therapy for better bone density. We need to figure out something to ensure that this does not become a new pattern. And honestly, figure out how to help her bone to heal while she is also still critically ill.
I also had an appointment today with Urology. They would like Aimee to be seen by the surgery clinic for botox injections to allow to void urine without so many catheters. These serious repeated urinary tract infections have now culminated in sepsis, pancreatitis, and small intestine shut down. This cascade of events has definitely changed my perspective on using the botox. I had previously been avoiding it as it must be repeated under sedation every few months.
No wonder Aimee is overwhelmed.
10.13.21 ICU 20
This has been an increasingly difficult 24 hours. Aimee is stable again at the moment.
The episodes that we were seeing the night before became more and more frequent throughout yesterday. It started only when we would do positioning, then anytime we had to suction or touch her, then it became constant. Despite many extra boluses of anxiety and pain meds, she spent hours last night spasming and shaking. She had consults all over the place, x-rays, blood draws, many different meds, and finally had an added dose of diazapam with rescue dose of atovan. She seemed to be neurologically storming. Her eyes were going crazy, her whole body was shaking, she was grimacing, and pulling her head back. Her sats were intermittently bad and she was on high oxygen and had diminished lung sounds. It was all happening at once and we are so grateful to be here where things can happen quickly when they need to happen quickly.
Neurology gave her an increased, loading dose during the night of the IV seizure med with plans for her regular daily doses to be increased based on the blood levels taken last night. The thought is to also add a drip of atovan along with the dilaudid drip and the precedex drip.
In other news, all of that movement seems to have adjusted the position of the trach, which is making it difficult to get air in and out of her lungs. Early this morning the Otolaryngology doctor checked over her from the outside and it seems that the position of the trach may have shifted against the back wall of her trachea. In a few minutes they will be doing a scope here at bedside. Getting a small amount of anesthesia ready.
General surgery just left after repacking her abdominal wound. It looks clean and healthy to me, but is disconcerting to have an open wound hanging around. They keep trying to stop the suction of her stomach and it ends up becoming distended within a few hours. Planning to try turning off suction again this afternoon to see if she can handle it.
This is hard. Aimee is being so brave, but her body is going through a lot. The process has not been as smooth as everyone thought it would be. We are praying that she stays strong, that she is able to have healing rest with the extra medications on board.
10.12.21 ICU 19
Aimee has a broken leg!! On top of everything else going on in her body. 2 weeks ago she had a shower at home with no noted events, but ever since that time she has been really sensitive about her leg being moved and holds it in a different position. I brought it up to her nurses here many times to ask that they be careful moving it. I thought that she probably pulled a muscle or that her hip was hurting, but yesterday I noticed the knee was more swollen and somewhat warm. They did an x-ray this morning and sure enough it is broken above the knee joint. 😩 Orthopedics will be putting a knee brace on to immobilize it. I am hopeful that she will feel a lot more secure and less stressed with turns. She is known to be at a higher risk for fractures, but this is our first experience with normal cares causing one.
This morning general surgery came to repack her open abdominal wound. It looks clean and healthy after yesterday’s procedure. They will be leaving it open and repacking it twice a day as it hopefully heals back up.
Also, she had a tough night with several extra boluses of dilaudid on top of her drip. She is easily startled and begins panicking with movement. It seems like she thinks she is choking. There is a difficult play right now between keeping her sedated and keeping her lungs in the best shape. The team keeps vacillating between using things like cough assist to keep her lungs open or not using it to avoid trauma to her fresh trach. The two sides of the argument finally came to an agreement this afternoon. We will only use cough assist if we absolutely have to and can’t clear her lungs. Otherwise we will do chest PT with the vibes every 6 hours to keep her lungs as open as possible. Hoping that this will be enough as she has had multiple events of thick secretions causing desats this morning.
10.11.21 ICU 18
Such a tough evening for Aimee. Despite sedation and pain meds, she panics with movement and violently shakes. Even her eyes are shaking. It is horrible. Praying that the increase in meds allows her to rest tonight and that her lungs stay clear on their own. They have had to do respiratory treatments every 4 hours up until now and we hope that none will be needed tonight. Cough assist would be very distressful right now. 💔
10.11.22 ICU 17
Alright. She is back with us. Surgery went well. It is wonderful to see her cute face. 
Apparently her trachea was off of midline, so they put in a smaller size than normal for her age/size. She also had a different presentation in that her trachea did not have rings like a normal trachea. The surgeon felt that this is a genetic abnormality, but should not affect the care. She will be mostly sedated and on pain meds for a couple days. By Friday they will be able to do her first trach change. She will remain in the ICU for now.
Apparently her trachea was off of midline, so they put in a smaller size than normal for her age/size. She also had a different presentation in that her trachea did not have rings like a normal trachea. The surgeon felt that this is a genetic abnormality, but should not affect the care. She will be mostly sedated and on pain meds for a couple days. By Friday they will be able to do her first trach change. She will remain in the ICU for now.
While she was in the OR the general surgery team opened up part of her abdominal incision. There was some infection. They cleaned it out, took cultures, and packed the wound. This would most likely explain the fevers she has been having throughout the week. Her belly looks softer, but we expect that her gut will stay slow with sedation for now. She will continue to be fed via TPN and to have her stomach drained/suctioned.
FYI: Aimee was moved to Forest 5 room 201. Still ICU.
10.11.21 Trach Surgery
Aimee just left to the OR for her trach surgery, which should only be about 2 hours. 


We are empty nesters for the moment as we wait.
We are empty nesters for the moment as we wait.
10.10.21 ICU 16
We were able to decrease the IV seizure medications that neurology has Aimee on two days ago and she has perked up a bit since then. Unfortunately with a bit of feistiness, she is starting to panic and think she is choking on the breathing tube. Very hard to see and to help her stop fighting it. Today they added an IV drip anxiety med and it is so far decreasing her heart rate and allowing her to be more calm. Still starting getting some eyes here and there thankfully. :) Especially for Ed. She is still and always a daddy’s girl. 




























Today Aimee has begun to have a bit of ostomy output. No air yet, so her belly is still full and still has suction pulling out anything from her stomach. But, some progress there is very encouraging and hopeful. We got results from her CT scan, which showed distended bowel loops, but no blockage or abscess. So, time. We have to be patient and wait for function to return. And hope that it fully will.
The attending did tell us that it is not unusual for bowel and bladder function to start declining as the respiratory system becomes more stressed in kids like Aimee. Essentially, she was telling us what the Neurodevelopmental doctor said a couple weeks ago… their systems get tired after working so hard to live. That is hard to accept and process, but also means we will focus on savoring life with Aimee as long as we can. We want to get her home to have as many happy moments, hopefully happy years, as we can together as a family.
Speaking of that goal, here is a photo dump reminder of happy moments with Aimee from the past couple of years:
Subscribe to:
Comments (Atom)